The Vagus nerve is the longest nerve in the body and an essential actor in the parasympathetic nervous system. It influences physical, mental, and emotional health and is associated with a strong, healthy immune response. When it comes to your body, your vagus nerve is involved whether you’re breathing, digesting, sleeping, or exercising.
Also known as the Wanderer Nerve, the vagus nerve travels from the brainstem down throughout the body innervating (controlling) many major organs. Vagal nerve dysfunction has been attributed to hundreds of health conditions—both chronic and acute. Understanding a bit about the vagus nerve can offer insight into how to better your health goals.
Table of Contents
Highlights
- The Vagus Nerve is the longest nerve system in the CNS
- It sends and receives signals to many major organ systems
- It regulates the sympathetic nervous system controlling sleep, digestion, and hormonal balances.
- The Gut-Brain connection (HPA Axis) communicates via the vagus nerve
- Vagus nerve health can be effectively measured and monitored via Heart Rate Variability (HRV)
- Vagus nerve dysregulation may play a role in nearly every chronic health condition
- There are common exercises and training routines that can help strengthen vagal tone and have a positive impact on a range of health conditions.
Introduction
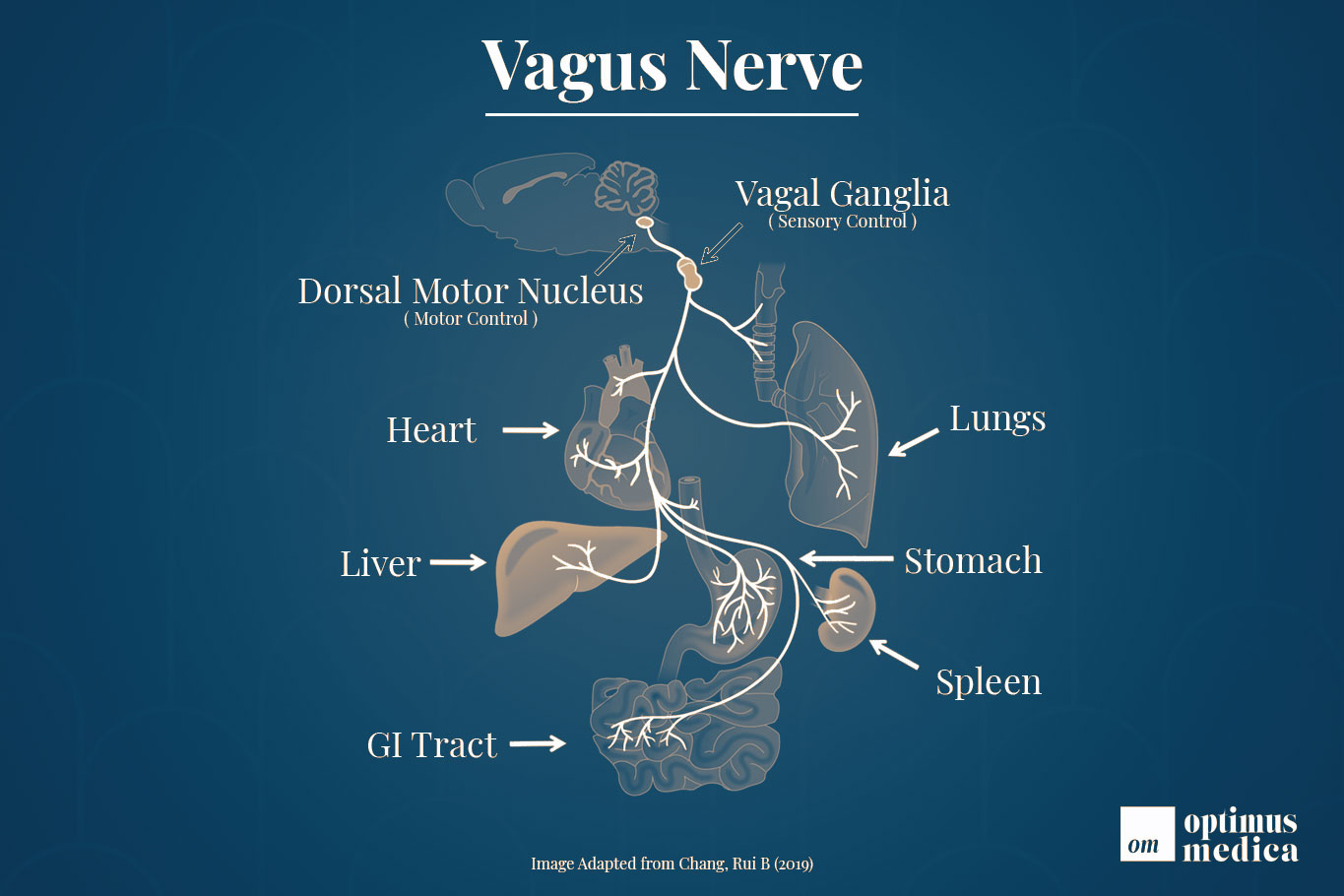
The vagus nerve is the longest network of nerve fibers in our central nervous system (CNS). It both receives and sends signals to and from many major organ systems and regulates the parasympathetic response. Its role in our health is immense—quickly being recognized by modern research—but not always simple to understand.
The health of one’s vagus nerve is referred to as vagal tone. This term is used throughout this article, as well as in medical texts, to describe the relative health and functionality of the vagus nerve. Higher vagal tone means better overall vagus nerve health while. Vagal tone is commonly measured by heart rate variability (more on that in just a second).
Low vagal tone has been associated with dozens, if not hundreds, of health conditions ranging from allergies all the way to cancer. Researchers have used HRV (and thus vagal tone) as a measure to accurately predict relative outcomes of patients suffering from similar conditions. Simply put; of two patients with a similar prognosis—the one with the higher vagal tone with fare better.
There are a number of measures one can take to both assess, measure, and improve vagal tone. These range from simple at-home breathing exercises and smartphone apps to extensive HRV monitoring systems and real-time imagining methods. This article provides an overview of the vagus nerve with links to additional resources for more detailed discussions when available—but first, some important terminology:
Afferent vs. Efferent
The CNS can be realized as including two types of neurons: afferent and efferent. Afferent neurons are responsible for receiving signals from the CNS. Efferent neurons are responsible for sending signals to the CNS. The vagus nerve contains both afferent and efferent branches thus allowing it to both serve as an observer-to and controller-of the CNS (10). I used the phrase A is for Action to distinguish the two.
Learn More: SEER’s Nervous System Training Module
Heart Rate Variability
Heart rate variability is the single most effective means of measuring vagal tone. Heart rate is the measure of how many beats-per-minute whereas HRV is the measure, generally in milliseconds, of the time interval between beats. Higher average measures of HRV indicate better vagus nerve health. This term is used throughout the remainder of this article to help describe the degree to which certain actions may (or may not) affect the vagus nerve.
Learn More: HRV Introduction by MindDrip (video)
Hypothalamic-Pituitary-Adrenal Axis (HPA)
The HPA axis—as its name implies—connects the hypothalamus, pituitary gland, and adrenal glands. The hypothalamus and pituitary glands are located near the brain stem and the adrenal glands sit just above the kidneys. The HPA axis helps control the body’s reaction to stress. The study of the vagus nerve, particularly its reaction to certain things like probiotics, involves the assessment of HPA function. The “Gut-Brain” connection often refers to the dynamics of HPA function.
Learn More: How Stress Affects the Brain (TED Talk, Video)
Assessing Vagus Nerve Dysfunction
It’s very conceivable one might want to assess their own vagal tone given the role the vagus nerve plays in health. There are a number of approaches to measure and assess vagal tone that ranges from simple at-home tests to complex diagnostic procedures requiring a medical professional. Below are a few of the most straightforward at-home assessments one can do.
- Head Lean
- Uvula Check
- Gag Reflex
Vagus Nerve Stimulation
Stimulating the vagus nerve is regarded as an effective means of increasing vagal tone. The term “vagal stimulation” includes a range of methods ranging from the simple gargling of water to using precision electronic frequencies.
Vagal stimulation has been studied for its relevancy in contexts ranging from boosting athletic performance, improving digestion, to major conditions such as metabolic syndrome and epilepsy (4). Below is a simplified overview of many ways in which the vagus nerve can be stimulated.
Cold Exposure
Exposure to cold temperatures activates the parasympathetic nervous system in ways that can help reduce inflammation. This type of hormetic therapy activates the vagus nerve and can lower inflammatory cytokines like IL-6 and increase anti-inflammatory compounds like IL-10 (5)(7).
In one randomized study, researchers found that cold exposure to a single area of the body was able to produce favorable vagal responses. These responses were measured in Heart-Rate-Variability and described positive outcomes related to the vagus nerve and heart (6).
Deeper Dive: Wim Hof Method’s Vagus Nerve Stimulation
Resonance Breathing
Resonance breathing is a breathing technique where one inhales and exhales for an equal amount of time. That is breath in for 5 seconds, breath out for 5 seconds. Resonant breathing is often referred to as diaphragmatic breathing but it’s not quite the same. Diaphragmatic breathing simply involves taking deep breaths whereas resonance breathing is a more synchronous exercise.
Research has shown that the simple act of slowing one’s breathing rate can have a positive impact on health conditions involving the parasympathetic nervous system, such as anxiety or depression (8). These positive changes can be measured as increases in HRV—again, reflective of increases in vagal tone (9). Resonance breathing techniques are clinically verified means of stimulating the vagus nerve and increasing HRV.
Deeper Dive: Heart Math & Coherence
Singing, Chanting, & Humming
Electro-stimulation of the vagus nerve is sometimes used to treat non-responsive epilepsy with decent success rates (11). One of the few side effects common with treatment is alterations in a patient’s voice (12, 13). The vagus nerve innervates the larynx via the afferent fibers but can also detect stimulation originating from stimulating the larynx as well.
Research has shown such activities as chanting, singing, and humming to increase HRV—thus improving overall vagal tone (14). Interestingly, exposure to certain types of sound has also been shown to improve vagal tone (15). This suggests that group singing, such as church choirs, may compound the benefits of vocal vagal toning by amplifying the influence of beneficial auditory tones.
Deeper Dive: Music Structure Determines HRV of Singers
Probiotics
The science behind probiotics is very much in its infancy. There are studies resulting in both positive and negative outcomes with probiotics. The byproducts of microbial and fungal metabolism are known to influence our CNS via interaction with the HPA (17, 18). Such interactions have been observed by certain probiotics causing or alleviating symptoms of anxiety and stress, increasing levels of certain neurotransmitters like GABA, Serotonin, and Norepinephrine, as well as mitigating symptoms of complex illnesses like Autism Spectrum Disorder (ASD).
The HPA access is sensitive to the activity of different microbial species. HRV has become a measure of interest for describing the metabolic effects of probiotics on human health. As we know, HRV is also the best measure of vagal tone. Probiotics have been observed to have such influence over mental and emotional health that some researchers have even adopted the term Psychobiotics to describe certain strains of beneficial bacteria (19).
Learn More: Gut-Brain Axis Modulation by the Vagus Nerve
Other Ways to Stimulate the Vagus Nerve
In addition to the methods of vagal stimulation mentioned above, the following methods have strong scientific support for their favorable impact on vagal tone:
- Frequency Specific Modulation
- Binaural Beats
- Meditation
- Omega-3 Fatty Acids
- Exercise
- Massage
- Laughing & Socializing
Cranial Nerves
The Vagus nerve is the 10th cranial nerve, denoted in medical texts as CN X (C-cranial, N-Nerve, X-Ten). The Vagus nerve is actually a pair of nerves, referred to as the afferent (right) and efferent (left), which run along the body on both sides.
The autonomic nervous system is made of three primary components: the sympathetic, parasympathetic, and enteric nervous systems. The vagus nerve plays an integral role in each—regulating everything from our gut health, heart health, and emotional wellbeing (1).
The vagus nerve is the central hub of the hypo-pituitary axis (HPA) and carries signals between the gut and brain. Through this role, the nerve helps regulate inflammation throughout the body while also regulating immune responses (2).
The vagus nerve originates in the brainstem and from there extends down the neck and thorax all the way to the abdomen. It this wide-reaching span, and somewhat meandering path to get there, that the Vagus nerve has been dubbed the wandering nerve among many medical texts (3). Truly—the role the vagus nerve plays in regulating the nervous system is extensive.
Regulation
The vagus nerve plays a tremendous role in regulating a range of systems in our bodies. Research continues to emerge indicating the vagus nerve’s role is even more involved than previously realized. Traditionally, the vagus nerve is recognized as having an influential role in the following aspects of our bodies:
- Voice, Swallowing, & Hiccups (24)(25)
- Heartbeat Regulation (27)
- Gut Motility & Digestion (20)
- Enzyme & Bile production (23)
- Neurotransmitter production (22)(26)
- Nausea, Vomiting, & Stomach Acid production (21)
Review
The Vagus nerve is arguably the most influential nerve system in the human body. It regulates the nervous system; enervating organs ranging from the heart to the gastrointestinal tract. The stronger vagal tone has been connected to better health in many cases and dysregulation of this nerve may play a role in nearly every major disease. While this article is far from comprehensive of all one should consider regarding the vagus nerve, I hope that it helps convey the importance this nerve serves in understanding modern health concerns.
References
- Carabotti, Marilia et al. “The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems.” Annals of gastroenterology vol. 28,2 (2015): 203-209. PMID: PMC4367209
- Rosas-Ballina, M., et al. “Acetylcholine-Synthesizing T Cells Relay Neural Signals in a Vagus Nerve Circuit.” Science, vol. 334, no. 6052, 2011, pp. 98–101. doi:10.1126/science.1209985.
- Clancy, Jennifer A et al. “The wonders of the Wanderer.” Experimental physiology vol. 98,1 (2013): 38-45. doi:10.1113/expphysiol.2012.064543
- Howland, Robert H. “Vagus Nerve Stimulation.” Current behavioral neuroscience reports vol. 1,2 (2014): 64-73. doi:10.1007/s40473-014-0010-5
- Muzik, Otto, et al. “‘Brain over Body’–A Study on the Willful Regulation of Autonomic Function during Cold Exposure.” NeuroImage, vol. 172, 2018, pp. 632–41. doi:10.1016/j.neuroimage.2018.01.067.
- Jungmann, Manuela et al. “Effects of Cold Stimulation on Cardiac-Vagal Activation in Healthy Participants: Randomized Controlled Trial.” JMIR formative research vol. 2,2 e10257. 9 Oct. 2018, doi:10.2196/10257
- Chang, Rui B. “Body thermal responses and the vagus nerve.” Neuroscience letters vol. 698 (2019): 209-216. doi:10.1016/j.neulet.2019.01.013
- Zautra, Alex J et al. “The effects of slow breathing on affective responses to pain stimuli: an experimental study.” Pain vol. 149,1 (2010): 12-18. doi:10.1016/j.pain.2009.10.001
- Strauss-Blasche, G et al. “Relative timing of inspiration and expiration affects respiratory sinus arrhythmia.” Clinical and experimental pharmacology & physiology vol. 27,8 (2000): 601-6. doi:10.1046/j.1440-1681.2000.03306.x
- Uvnäs-Moberg, K. “Role of efferent and afferent vagal nerve activity during reproduction: integrating function of oxytocin on metabolism and behaviour.” Psychoneuroendocrinology vol. 19,5-7 (1994): 687-95. doi:10.1016/0306-4530(94)90050-7
- Krahl, Scott E. “Vagus nerve stimulation for epilepsy: A review of the peripheral mechanisms.” Surgical neurology international vol. 3,Suppl 1 (2012): S47-52. doi:10.4103/2152-7806.91610
- Charous, S J et al. “The effect of vagal nerve stimulation on voice.” The Laryngoscope vol. 111,11 Pt 1 (2001): 2028-31. doi:10.1097/00005537-200111000-00030
- Charous, Steven J., et al. “The Effect of Vagal Nerve Stimulation on Voice.” The Laryngoscope, vol. 111, no. 11, 2001, pp. 2028–31. Crossref, doi:10.1097/00005537-200111000-00030.
- Vickhoff, Björn et al. “Music structure determines heart rate variability of singers.” Frontiers in psychology vol. 4 334. 9 Jul. 2013, doi:10.3389/fpsyg.2013.00334
- Ellis, Robert J, and Julian F Thayer. “Music and Autonomic Nervous System (Dys)function.” Music perception vol. 27,4 (2010): 317-326. doi:10.1525/mp.2010.27.4.317
- Vickhoff, Björn et al. “Music structure determines heart rate variability of singers.” Frontiers in psychology vol. 4 334. 9 Jul. 2013, doi:10.3389/fpsyg.2013.00334
- Appleton, Jeremy. “The Gut-Brain Axis: Influence of Microbiota on Mood and Mental Health.” Integrative medicine (Encinitas, Calif.) vol. 17,4 (2018): 28-32. PMID: 31043907
- Carabotti, Marilia et al. “The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems.” Annals of gastroenterology vol. 28,2 (2015): 203-209. PMID: 25830558
- Bermúdez-Humarán, Luis G et al. “From Probiotics to Psychobiotics: Live Beneficial Bacteria Which Act on the Brain-Gut Axis.” Nutrients vol. 11,4 890. 20 Apr. 2019, doi:10.3390/nu11040890
- Browning, Kirsteen N et al. “The Vagus Nerve in Appetite Regulation, Mood, and Intestinal Inflammation.” Gastroenterology vol. 152,4 (2017): 730-744. doi:10.1053/j.gastro.2016.10.046
- Babic, Tanja, and Kirsteen N Browning. “The role of vagal neurocircuits in the regulation of nausea and vomiting.” European journal of pharmacology vol. 722 (2014): 38-47. doi:10.1016/j.ejphar.2013.08.047
- Browning, Kirsteen N. “Role of central vagal 5-HT3 receptors in gastrointestinal physiology and pathophysiology.” Frontiers in neuroscience vol. 9 413. 29 Oct. 2015, doi:10.3389/fnins.2015.00413
- Li, Y, and C Owyang. “Vagal afferent pathway mediates physiological action of cholecystokinin on pancreatic enzyme secretion.” The Journal of clinical investigation vol. 92,1 (1993): 418-24. doi:10.1172/JCI116583
- Hanks, Geoffrey, et al., eds. Oxford textbook of palliative medicine. Oxford university press, 2011.
- Becker, Daniel E. “Nausea, vomiting, and hiccups: a review of mechanisms and treatment.” Anesthesia progress vol. 57,4 (2010): 150-6; quiz 157. doi:10.2344/0003-3006-57.4.150
- Porges, Stephen W., Jane A. Doussard-Roosevelt, and Ajit K. Maiti. “Vagal Tone and the Physiological Regulation of Emotion.” Monographs of the Society for Research in Child Development 59, no. 2/3 (1994): 167-86. Accessed May 30, 2021. doi:10.2307/1166144.
-
Levy, M N et al. “Assessment of beat-by-beat control of heart rate by the autonomic nervous system: molecular biology technique are necessary, but not sufficient.” Journal of cardiovascular electrophysiology vol. 4,2 (1993): 183-93. doi:10.1111/j.1540-8167.1993.tb01222.x